Interview with Taylor Davis, CareLuminate Founder, Consultant
“I would be in different hospitals and think this place is truly scary in terms of the quality of care. A lot of times patients would not see the Russian Roulette decisions being made behind the scenes with their health.”
– Taylor Davis
Sounding the Alarm on the Hospital Quality Crisis
Taylor Davis knows an ugly healthcare secret, and he wants to spread the word. Years spent in hospitals researching health IT taught him that 1) the level of quality and safety ranges widely between hospitals and 2) patients have no idea.
“There is huge variation in quality of care between hospitals. Your average American thinks a hospital is a hospital and that the big variation is the physician, and that is not true,” he explains. “The physician is a variation point but hospitals are a huge variation point.”
Taylor spent most of his career consulting in health IT. During his tenure, Taylor’s firm interviewed hundreds of thousands of clinicians, and Taylor spent a lot of time observing practices in hospitals both in Utah where he lives and across the country. These experiences gave him a behind-the-scenes view of quality of care.
“I would be in different hospitals and think this place is truly scary in terms of the quality of care,” he recalls. “A lot of times patients would not see the Russian Roulette decisions being made behind the scenes with their health.”
A nurse who served as her hospital’s operating room manager recounted one such decision to Taylor. Her facility ran out of DuraSeal, a sealant used with sutures to repair tears caused by surgery to the dura, the lining around the spinal cord that prevents cerebrospinal fluid from leaking. You can think of DuraSeal as spine surgery insurance – if there is no tear, it is not used, but if there is a tear it is an important material to have on hand to prevent a range of neurological complications for patients. The hospital instructed the nurse to continue to book spine surgeries even though the hospital was out of DuraSeal, she pushed back, and ultimately the hospital went forward booking and then performing the surgeries. The hospital later claimed that DuraSeal had been on-hand the whole time, but the nurse disputes this. The patients operated on likely were not aware of this exchange.
Incidents of poor quality in hospitals range from simple apathy toward patient discomfort to life ending medical mistakes. Taylor pinpoints understaffing as the main driver across the board. Bedbound patients in hospitals need to be manually turned, but hospitals often do not invest in enough lift mobility aids and due to staff shortages, patients are left to gather bed sores. Patients are kept sitting in their own waste and often bathed only once every three days. Most alarmingly, ICU nurses have told Taylor about having to treat five patients at a time, when two patients would be a typical ICU caseload.
“When you are stretched that much, you are going to make mistakes. It is a vicious cycle because hospitals are asking nurses to do more than they should. You have nurses that are exhausted, overworked during shifts, taking on more patients than anyone should, they make a mistake, a patient dies, the nurse leaves healthcare, and now healthcare is down another clinician,” Taylor explains.
The Health Resources and Services Administration projects a shortage of almost 79,000 full-time registered nurses (RNs) by 2025. While America’s aging workforce feeds into the shortage, there has also been an alarming trend of nurses leaving bedside practice following the Covid-19 pandemic. A 2022 Health Affairs study led by Dr. David Auerbach found that there was a decline of over 100,000 RNs in the United States from 2020 to 2021, the largest recorded drop in the nursing workforce documented in the past 40 years.
Low Quality, High Price
Hospital closures are a growing issue in much of the country, especially in rural communities where they not only hinder healthcare access but equate to the loss of a major employer. The national healthcare expenditure has also ballooned to a whopping $4.5 trillion as of 2022, with hospital care accounting for 30% of the bill per Kaiser Family Foundation analysis. So how can the dual realities of high healthcare spending and financially insolvent hospitals closing exist, and how does this affect quality of care?
“Today insurance does not pay hospitals based off quality of care. Insurance pays based off the hospital’s ability to negotiate. Insurance can miss one hospital here or there, but they cannot miss a big health system,” Taylor explains.
Commercial insurance dynamics favor larger hospital chains, which have greater leverage to negotiate for higher reimbursement rates. Additionally, Medicare and Medicaid pay hospitals lower rates than commercial equivalents. Therefore, hospitals caring for more older or low-income patients fare worse financially, especially if they are also independent and reimbursed at lower rates from commercial plans.
“Some hospitals heroically give care with little funding. Other hospitals’ financials do not look good because they are poorly managed and others are incredibly flush with cash,” Taylor describes. “You cannot treat those all the same, but when you come down to hard decisions about how we do not have enough money to give the type of care we want, Americans do not go home for the holidays like they could have.”
Shedding Light on Quality: The CareLuminate Story
Despite witnessing hazardous incidents and hearing directly from hospital staff that they believed their hospital had poor quality, Taylor noticed that even the worst hospitals still had positive public-facing quality metrics.
“We have corporatized healthcare so much that we expect that if you do not like the quality, you can go elsewhere. The problem is that you do not know what the quality is in hospitals until you or your family member are naked under a sheet on an operating table, and at that point it is very hard to switch,” Taylor summarizes.
“I felt passionate that there needs to be a metric that hospitals cannot manipulate that helps people know what they are actually going to get when they go into a hospital: is it going to be good care or bad care,” he explains.
Taylor founded CareLuminate in 2023 to bring transparency to hospital quality of care through what he describes as Upton Sinclair-style investigative reporting. CareLuminate captures feedback from large samples of frontline nurses through surveys and interviews about where they would recommend their loved ones seek care as well as incidents where they have witnessed poor quality care. While the studies include some physicians, the organization believes that nurses offer the best perspective into quality practices because of their frontline, bedside role. CareLuminate currently has completed studies in five cities across America and is working on a large national oncology care study. Results of all studies are publicly available, providing valuable insights to patients and caregivers.
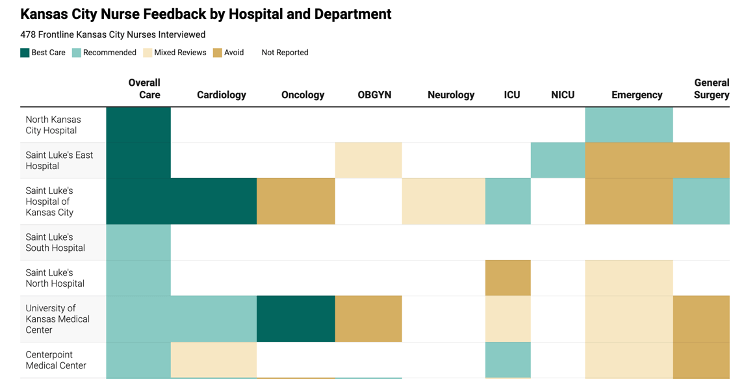
Source: Excerpt from 2023 Kansas City Healthcare Quality Guide, CareLuminate.
Utah: A Great Place to Live
Taylor views both the poor quality of care in hospitals and the lack of transparency surrounding it as national issues. He has not yet completed a CareLuminate study in Utah where he resides, but Utah trends toward having strong healthcare performance overall. In fact, many major metrics are positive for Utah (population: 3.4 million) to the extent that the southwestern state recently earned the top spot for the 2024 US News state rankings for the second year in a row.
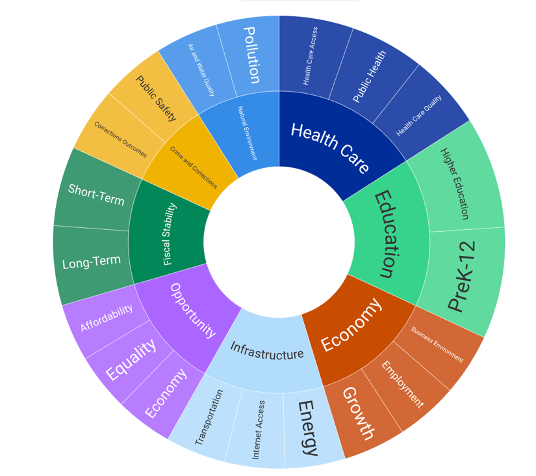
Source: US News Best States 2024: How They Were Ranked, May 2024.
“I love the state. It is a really good place for healthcare and a more affordable care location,” Taylor notes. “The recreational opportunities in Utah are also phenomenal – skiing in winter, hiking in summer. It is a great place to live, and it has gotten expensive because people have realized it is a great place to live.”
Utah is beautiful. Southern Utah is full of vibrant warm toned desert landscapes, cliffs, and canyons. Northern Utah is full of snowcapped mountains and the Great Salt Lake that gives the capital its name. The state also has the “Mighty Five” national parks, which each offer distinct geological features from emerald waterfalls below sandstone cliffs in Zion to spiraling limestone hoodoo formations in Bryce Canyon.
Within healthcare, Intermountain Health, University of Utah Hospital, and the Huntsman Cancer Institute are all considered to be on the national forefront for their various key programs. In 2024 Fortune Magazine ranked Intermountain as the top large American healthcare system. All three hospitals are headquartered in Salt Lake City (population: 205,000), anchoring many healthcare companies like the consultancy Taylor worked for to the area. Taylor resides in American Fork (population: 37,000) about a half-hour drive south from Salt Lake City and twenty minutes north of Provo (population: 114,000).
Provo is best known nationally as the location of Brigham Young University (BYU), a private university operated by the Church of Jesus Christ of Latter-day Saints and the largest religious university in the country. Attending college at BYU initially brought Taylor, who is a member of the Church, to Utah after growing up in Southern Idaho. He went on to earn an undergraduate degree in economics as well as a master’s of business administration from BYU, breaking for a master’s in applied statistics from Texas A&M in between.
The Church of Jesus Christ of Latter-day Saints has had a significant presence in Utah since migrating to the region in the late 1840s. In 2022, ~40% of Utah residents identified as Church members; comparatively, ~72% did in 1970. Church practices continue to impact the state’s culture, including its health behaviors.
“Practicing members of the Church of Jesus Christ of Latter-day Saints do not drink coffee or alcohol and only take prescription drugs – no recreational drugs. It is not a solve-all, but it has done good things for the health of people in our community. If you can largely eliminate alcohol, smoking, and drugs, it creates more of a health focus in some ways,” Taylor shares.
Data supports this assessment. Utah’s rates of self-reported heavy and binge drinking are lower than the national average. The state ranks 49th in the nation for drunk driving incidence and deaths per Forbes. Similarly, Utah ranks 44th in the nation for drug overdose mortality rate, meaning the state has some of the lowest rates per the CDC.
A Quality Roadmap for Patients and Caregivers
Like many issues in healthcare, poor quality hospital care is a national versus state-specific concern. Even though Utah hosts some top Centers of Excellence, Taylor also suspects that some of the state’s hospitals have poor quality outcomes as well. Quality metrics can also differ within a hospital system – for example, showing positive metrics for labor and delivery but poor outcomes in cardiology within the same hospital.
For those of us living outside the five areas where CareLuminate has piloted studies, it may seem daunting to try to determine where to seek care for ourselves or loved ones, especially knowing that many truly dangerous quality decisions occur out of view. While Taylor works on expanding CareLuminate to provide quality transparency nationally, he recommends that patients and caregivers try their best to solicit their own recommendations from any clinicians they know. He also understands that this may be impossible for some.
“It is hard to navigate this horrible system, and typically if people navigate it successfully, it is because they have guidance from a practicing clinician. However, that also creates health disparities and inequities based on who does and does not have as much access to inside information,” Taylor highlights.
“Understaffed hospitals are a silent killer,” he summarizes. “Almost no one is focused on it, and clinicians cannot publicly speak out about it. Because of tort laws, no one tells you that the hospital cut corners, so you are in a situation where lots of Americans die and families think people were nice to me, I think care was good, but they do not realize corners were cut.”
CareLuminate allows nurses to speak out about quality of care by providing the anonymity and protection of being one interview or survey response among thousands. Having behind-the-scenes insights about the true level of care delivered in a hospital will hopefully be the first step in a longer-term shift to fix the pervasive issues in healthcare that are causing slipping quality in the first place.




Leave a comment