Interview with Dr. Courtney Younglove, Obesity Medicine Physician, Obstetrician-Gynecologist, Writer, and Policy Advocate
“We are trying not to take the limited approach of ‘just eat less’ and giving patients medicine to suppress their hunger hormones because that is a very temporary fix. It puts all your chips in the basket of your medications. Lots of people stop the medications because of the cost. I have patients all the time who say I do not want to take GLP-1s indefinitely, and I say I don’t want you to either, but we have to change the other things that got you here. So, we have to work on the lifestyle stuff, but that is really, really hard for most people.”
– Dr. Courtney Younglove
The Advent of Obesity Medicine
In 2005, when Dr. Courtney Younglove began working as a newly minted obstetrician-gynecologist (OB-GYN) in a Kansas City suburb, 24% of American adults had obesity. By 2023, 40% had obesity.
“My patients were coming in asking about weight, and I have had excess weight since I was twelve, so I was like, ‘hell if I know, this is what I’m doing this month.’ I felt very helpless that I wasn’t helping my patients and at the same time we were seeing more and more complications in obstetrics and gynecology related to excess weight. The amount of gestational diabetes, hypertension, and preeclampsia was climbing, and we were all scratching our heads and looking at each other,” she recounts.
Courtney is a third-generation physician and spent the first fifteen years of her medical career working at the practice her OB-GYN father had founded.
Courtney sought out a one-day educational session about obesity medicine led by the American Society of Bariatric Physicians, now the Obesity Medicine Association. She intended to leave with key learnings that she could weave across the OB-GYN clinic but instead encountered a full and exciting field of medicine. While continuing to practice as an OB-GYN, Courtney studied obesity medicine in depth and in 2015 sat for a board exam – only the ~800th physician to be board certified in the emerging field (now there are over 8,000).
“The overlap between women’s health and obesity medicine is my biggest passion. Anovulation, or not ovulating or not ovulating enough, is often driven by metabolic health, so fixing metabolic health should be a key piece of fixing ovulation, but most OB-GYNs do not know that, nor do they have the capacity to do that on top of everything. So many pregnancy and postpartum complications are related to metabolic health and obesity. There is an overlap with obesity and gynecologic cancers, breast cancer, and endometrial cancer. Women’s health and obesity medicine are so tightly woven together,” Courtney explains.
As Courtney practiced obesity medicine within the OB-GYN clinic, she quickly encountered practical constraints. She was the only physician trained to practice obesity medicine in the clinic, so she needed to see any patients seeking this care, but also had to occasionally run out to deliver babies. Simultaneously, she had to stay up to date with two fields of medicine. In 2018, Courtney decided to narrow in and founded independent obesity medicine clinic Heartland Weight Loss in Overland Park (population: 203,000), Kansas (population: 3M).
The GLP-1 Boom
Overland Park is a twenty-minute drive to Kansas City, an area that Courtney considers a well-kept secret within America despite the pop culture spotlight fixated on a certain recently engaged football player and singer. The McDonald’s Happy Meal, bumper stickers, and Hallmark all got their start in what has been nicknamed “the Paris of the Plains.”
Kansas City also faces a unique paradox where the Kansas-Missouri state line runs through the metropolitan area, resulting in two distinct cities: Kansas City, Kansas (population: 157,000) and Kansas City, Missouri (population: 516,000). As a Kansas-accredited physician, Courtney is restricted to only provide care on her side of the Missouri River.
Kansas holds the geographic center of continental America. Perhaps influenced by this, the state has had a long history of aviation manufacturing; coincidentally, aviation pioneer Amelia Earhart was a Kansan. And yes, the band Kansas, of “Carry On Wayward Son” and “Dust in the Wind” fame, is from Kansas.
According to 2023 CDC data, 36% of adults in Kansas have obesity, giving the state the fifteenth highest obesity rate out of the 48 states reporting data.
At Heartland Weight Loss, Courtney and her team take a holistic approach to care for patients, emphasizing stress management, sleep tracking, nutritional counseling, and exercise to maintain muscle composition. In addition to these lifestyle pillars, many of Courtney’s patients also utilize medication to assist their weight loss journeys.
“At the beginning, we were using some of the GLP-1s off-label since they were FDA approved only for diabetes at the time,” Courtney recalls. “We had a lot of patients who were diabetic using them, so we were comfortable with the medications. Then they all exploded on social media and the whole world turned upside down.”
In 2021, Ozempic became the shot heard round the world.
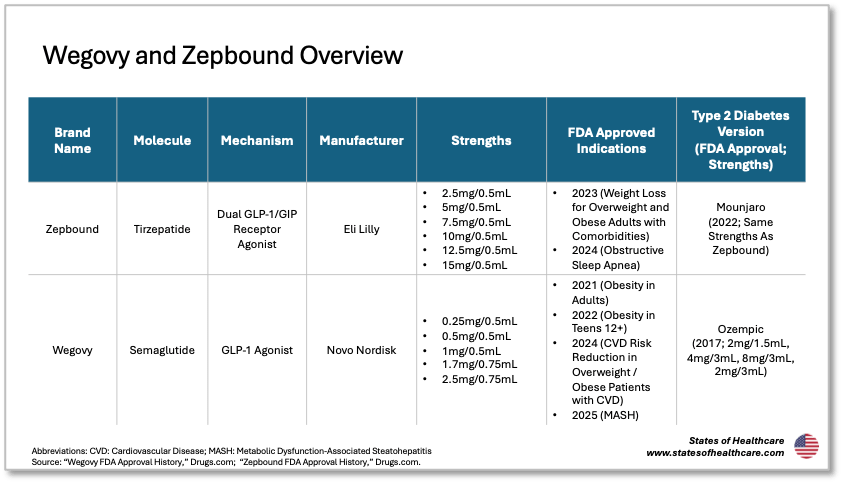
Ozempic is a weekly injected glucagon-like peptide-1 (GLP-1) and was approved by the FDA in 2017. Although Ozempic is a household name synonymous with weight loss, and a catchy jingle, it is specifically approved for use by people with Type 2 diabetes seeking to control their blood sugar. Wegovy, which the FDA approved in 2021, is the same molecule from the same manufacturer but indicated for weight loss. This distinction is important and introduces lots of nuances related to access and affordability.
GLP-1s were popularized for weight loss in 2021 but have been available since 2005, although most GLP-1 products have historically helped control blood sugar for Type 2 diabetics.
Jeffrey Friedman’s 2024 paper on the discovery and development of GLP-1 drugs summarizes the scientific timeline that led to the medication’s commercialization. GLP-1 is an incretin, or a hormone that stimulates the body to make insulin and was discovered in 1986. Novo Nordisk, already the world’s largest insulin manufacturer, began to investigate GLP-1 as a treatment for diabetes and obesity in the late 1990s. Simultaneously, researcher and physician John Eng, who was studying peptides in the venom of Gila monsters, identified a novel peptide similar to human GLP-1 but with a longer half-life; this discovery led to a collaboration that brought forth the first GLP-1: Byetta. The Novo Nordisk team eventually brought forth Victoza and Saxenda and continued to investigate how to make a once-weekly version, eventually leading them to create Ozempic and Wegovy.
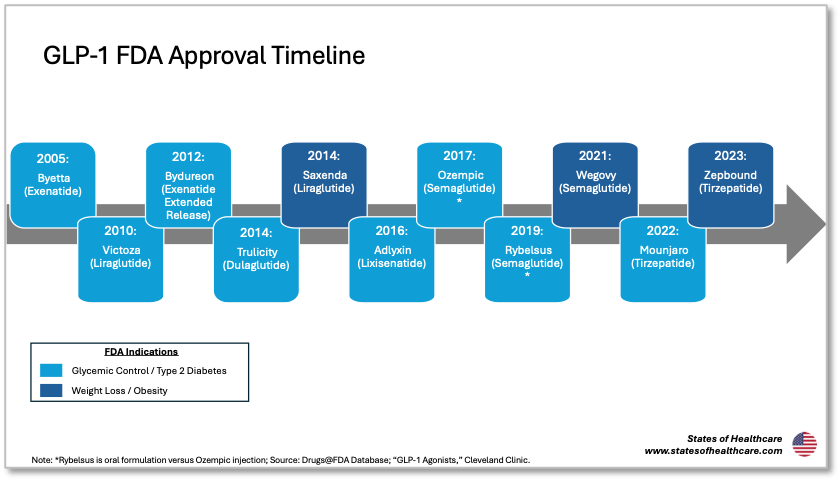
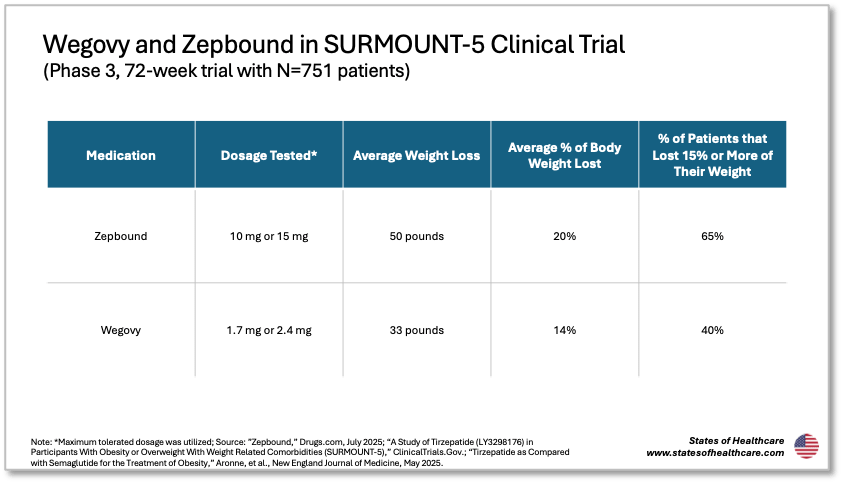
In 2023, dual GLP-1/GIP medication Zepbound gained approval for weight loss. Similar to the Ozempic dynamic, manufacturer Eli Lilly’s therapy Mounjaro had been available for Type 2 diabetics since 2022. In the SURMOUNT-5 clinical trial, patients utilizing Zepbound lost 50 pounds on average compared to the 33 pounds that patients utilizing Wegovy lost.
The Big Insurance Breakup
When Courtney founded Heartland Weight Loss, she wanted her services to be accessible, so she accepted insurance. As the GLP-1 boom unexpectedly ballooned plan spending for some insurers, a major commercial insurer in her area stopped reimbursing obesity medicine.
“They started denying every claim that we submitted that mentioned the word obesity, even if we were diagnosing diabetes or managing hypertension. The services were already performed and built into our budget. It was devastating to our patients, and it was financially devastating to us to lose that revenue,” Courtney recounts. “So we did a full turnaround and moved those patients to a self-pay system. We tried to straddle the fence for a year where we would bill other major insurers and then have patients under that one insurer self-pay, and that was really complicated. We could not do it without breaking, so we went to a full self-pay model also knowing that the other insurance agencies could stop reimbursing us at any time like the first plan had done. So we are a self-pay model, and a much smaller practice now than in 2018.”
Heartland Weight Loss charges patients $225 for their first appointment and $165 monthly for follow-up visits.
Most insurers cover GLP-1s when used to manage Type 2 diabetes (i.e., they cover Ozempic but not Wegovy). Medicare has historically not paid for medications that support weight loss, explicitly listing this group in a small group of carved-out medications. In 2024, the Biden Administration proposed allowing Medicare and requiring Medicaid to cover anti-obesity medications, and in June 2025 the Trump Administration rejected this proposal.
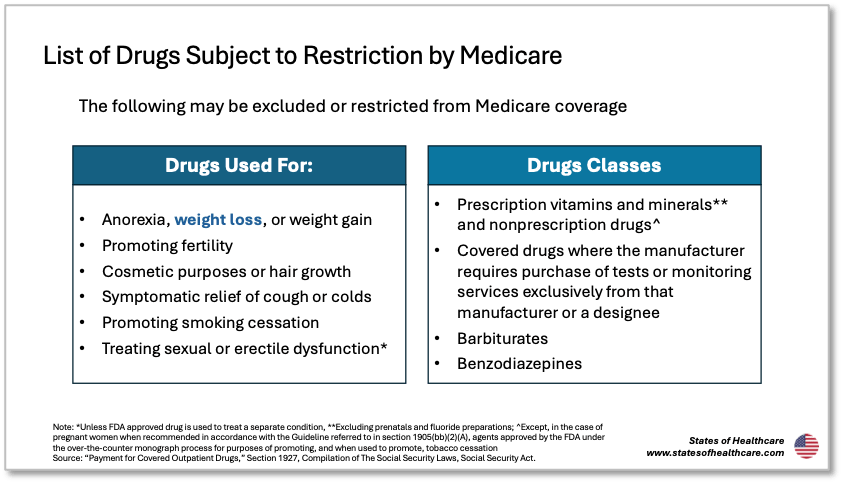
“Commercial insurers take their cues from Medicare. When Medicare says we will not do this, private insurers do the same. If we got rid of the prohibition on Medicare covering anti-obesity medications, commercial insurers would face a lot more friction in refusing to cover this,” Courtney adds.
A 2024 Congressional Budget Office report estimated that Medicare coverage of anti-obesity medications would cost $35 billion from 2026 to 2034.
Cascading Concerns: Access, Off-Label Use, and Compounding
In addition to affordability concerns, access to GLP-1s quickly became a challenge. As supply shortages reigned, wealthy Americans paid up to obtain what became nicknamed “Vitamin O.” Notably, many patients with Type 2 diabetes struggled to get their prescribed GLP-1s due to the shortages, spurring criticism of celebrity and influencer promotion of off-label use of the medications.
In June 2024, Eli Lilly released a statement advising against the use of GLP-1 drugs for “cosmetic weight loss.” The statement noted that the therapies were meant to treat “serious diseases” and should not be used outside of their FDA-approved indications.
“The people who use GLP-1s for weight loss off-label and only have fifteen to twenty pounds of excess weight are losing muscle mass since they are typically not being monitored. When we see our patients lose muscle mass, we either turn down or turn off their medication because the last thing I want to do is create sarcopenia and osteoporosis, which accelerate death for aging women,” Courtney emphasizes. “Losing muscle mass is a disaster, especially in post-menopausal women. Building muscle for women after thirty is nearly impossible, so the goal should be to maintain what you have.”
Widespread off-label use of GLP-1s for aesthetically driven weight loss exacerbated shortages.
Semaglutide was placed on the official FDA shortage list between March 2022 and February 2025. Similarly, tirzepatide was on the FDA shortage list between December 2022 and October 2024.
Inclusion of these molecules on the FDA shortage list permitted compounding pharmacies to make their own versions of these medications despite them being newer drugs that are still patent-protected. Thus, e-pharmacy compounders like Hims / Hers and local brick-and-mortar medical spas, including medical spas on either side of the Heartland Weight Loss office, amplified the GLP-1 marketing deluge.
Courtney was initially curious about compounding since most of her patients could not access the new GLP-1 products otherwise. However, she was used to compounding drugs only in certain clinical cases, like to avoid an ingredient causing a patient sensitivity, versus compounding due to a shortage. She participated in an Obesity Medicine Association review of the practice and contributed to their publication on safe compounding.
“These medications were so inaccessible for most people, and they were so expensive. I am not opposed to compounding. I am used to compounded generics, where you buy the generic drug, put it in solution, and it’s all fine. But after 70 hours of research into compounding pharmacies and how they get the active pharmaceutical ingredients and the regulatory process, I was like we cannot do this. I am not going to put my name behind something that is not regulated. I am not going to put my patients’ safety at stake for ease of access,” Courtney outlines.
As detailed by researchers in a 2025 JAMA Health Forum piece, compounding pharmacies can reference the original brand medication’s safety and efficacy without demonstrating that their compounded version reaches these thresholds. In comparison, generic medications must demonstrate bioequivalence to the original branded medication to gain FDA approval. This and other regulatory nuances raise quality concerns related to compounding pharmacies.
Separate from these quality concerns regarding compounding, Courtney also felt uncomfortable selling drugs directly to her patients.
“My goal is never to profit from the sale of medicines. That is a conflict of interest in my mind and gross to me. As physicians, we should not profit because it does change your prescribing behaviors and that is not something I want to be part of, so we said no to compounding,” she explains.
Courtney works with patients to identify the best anti-obesity medications for their unique situation, considering clinical, cost, and access components.
“Not everyone needs a GLP-1. When my kids started having acne, I did not jump to Accutane; we started with the smaller guns,” Courtney details.
“We look with our patients at the list of anti-obesity medications, including the older oral drugs, and cross out what the patient cannot take for any medical reason. Then we talk about what to expect with each and the cost and side effects. It’s crazy that we have to talk about cost, but you have to in medicine. They can try one of the older oral medications, and if it is not working then we can step up to a GLP-1. If you are going to take a medication indefinitely or for years upon years, you do not want to start on something that costs $500 a month. The patients want to disengage with treatment when it’s expensive which can backfire when they are not ready.”
Courtney sometimes helps patients import brand Ozempic, Wegovy, Mounjaro, and Zepbound from established pharmacies in Canada and Israel, where they are often offered at lower prices than in the US for cash-paying customers. Now some of her patients also utilize Eli Lilly and Novo Nordisk’s direct-to-consumer purchasing option, a setup that health entrepreneur Halle Tecco describes as “pharm-to-table.” Novo and Lilly’s “pharm-to-table” offerings sell Wegovyand Zepbound respectively for $499 per month.
Creating Lifestyles for Lasting Change
Although social media gives the impression that GLP-1s are a miracle cure, the truth is a bit more complicated. A 2025 cohort study of over 125,000 patients initiating GLP-1s found that 47% of patients with Type 2 diabetes and 65% of patients without Type 2 diabetes discontinued use of the medications within a year, citing weight loss, income, and side effects from the drug as key drivers. 47% of the Type 2 diabetics and 36% of the non-diabetic patients reinitiated GLP-1s within a year, citing regained weight. This matters to Courtney.
“We are trying not to take the limited approach of ‘just eat less’ and giving patients medicine to suppress their hunger hormones because that is a very temporary fix. It puts all your chips in the basket of your medications. Lots of people stop the medications because of the cost. I have patients all the time who say I do not want to take GLP-1s indefinitely, and I say I don’t want you to either, but we have to change the other things that got you here. So, we have to work on the lifestyle stuff, but that is really, really hard for most people,” she explains.
“With medication assistance, patients can work on their lifestyle, and hopefully that lifestyle can become so foundational that you need less of the medications, knowing that you might need to restart them if your situation changes and you relapse. It is not a sexy approach, but it is a practical approach. The lifestyle should be strong enough to ideally anchor you. However, you can have a very solid, anchored lifestyle and still have the physiologic memory of obesity and it may want to come back. And things can disrupt it.”
Disruptions come in many shapes and sizes, but one big one for women? Menopause.
“Perimenopause is incredibly disruptive, with hormonal cycling, worsening insulin resistance, and sleep disturbances. We lose estrogen, which is a protector against hunger hormones and against insulin spikes. It is complex and overlaps with this midlife reckoning that women have that is also disrupting sleep, stress, purpose, and career. There are so many layers of midlife. It has been underappreciated for a long time, and women get gaslit a lot where people just say ‘here, take an antidepressant’ instead of addressing the underlying problems.”
Women in perimenopause are Courtney’s largest patient demographic and her favorite.
“Lots of patients want to lose the weight now and get healthy later. Women in their mid-forties and fifties are ready to buckle down and do the work,” she describes.
Despite the lean towards adult women, Heartland Weight Loss treats all types of patients, starting from age twelve, mirroring the current GLP-1 label.
Courtney treats older adolescents sometimes, but typically her nurse practitioner colleagues with family medicine backgrounds care for the younger patients. There is a large demand in the Kansas City area for pediatric obesity medicine, she notes, and the local children’s hospital has a program but with a very long waitlist. Courtney knows that this is a patient population with high unmet need and can empathize from some of her own experiences, having gone on Jenny Craig at fourteen and Weight Watchers at fifteen unsuccessfully.
“When these kids have this disease at age twelve, lifestyle interventions are almost ridiculously not helpful. It is so hard for that child to exist in a world that is very obesogenic around them. The standard treatment that most people approach obesity medicine with of ‘hey let’s just motivate you to eat less’ does not work. You have to eat differently, you have to think about mindset, you have to think about sleep and stress and all these other things. Asking a twelve-year-old to do that at a high level is really, really difficult, especially if the family situation is not set up in a way that they can do that,” Courtney explains.
“If we don’t treat these kids, they often are going to have severe obesity. Very few of them are going to spontaneously treat the disease themselves or grow out of it, which is what we used to think. They are going to enter their adulthood with a decreased life expectancy. Until we change the environment we raise these kids in, we have to give them what we can.”
For all patients, regardless of age, Courtney advises, “You have to have grace when your environment shifts and go okay, life is different, the pillars I put in place are not solid right now, but then you have to revamp it. That is the chronic nature of this. It happens to the best of people with the best health pillars, and we have to try to impart that on our patients. Yes, we can do all these things, but it is a fragile house of cards sometimes, so we need chronic disease management.”



Leave a comment